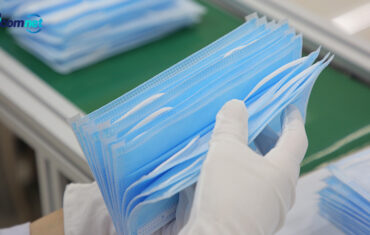
The current pandemic is reducing medical resources and requires PPE adaptation to the circumstances and to the scale of the threat to medical personnel. One should remember that it is the most important to follow the general recommendations on hand disinfection and the sequence of procedures when putting on and taking off PPE. It is essential to use masks with a filter, but also goggles and visors to protect the face, as well as double or triple gloves (Figure). Sterile surgical gloves are particularly useful as they are longer.
The optimal solution is to fully protect the entire body surface, isolate it from the environment, and breathe in air from a portable source, but this is not necessary in the case of SARS-CoV-2. At present, it is recommended to apply various types of equipment, including, in particular, partial protection of the environment through the use of surgical masks or ordinary face masks by persons with confirmed or potential SARS-CoV-2 infection; this may reduce the risk of infecting people in the environment, including medical personnel.
At present, performing a number of procedures in emergency medicine is associated with additional problems and risks for medical personnel. Emergency physicians, anesthesiologists and intensive care specialists, as well as the relevant scientific societies issue recommendations concerning endotracheal intubation or other procedures dangerous for the medical personnel. It should be remembered that endotracheal intubation by using direct laryngoscopy without adequate protection presents a high risk of SARS-CoV-2 infection.
The proposed modifications of endotracheal intubation include special preparation of the equipment and medical personnel, using a special protective box, foils applied to the upper half of the patient’s body, and the use of indirect laryngoscopy methods, including video laryngoscopy and rapid sequence intubation. In this context, it should be emphasized that attempts of prehospital endotracheal intubation by inexperienced personnel constitute a challenge, and supraglottic methods should be kept in mind.
If intravenous access cannot be established or is technically difficult, it is still possible to establish intraosseous access. Performing several procedures in protective clothing is technically difficult and exhausting, which is especially true for CPR. Certain intra-hospital procedures must be modified, for example, cardiopulmonary resuscitation in a patient with ARDS in a prone position and electrical defibrillation.
The COVID-19 pandemic poses a huge challenge for emergency teams, as well as physicians in emergency departments. The need for additional protection of the patient and medical personnel may result in a significant delay in the arrival of the emergency team, patient transport, and provision of intended medical care. During any pandemic, people still suffer from various diseases and injuries that require treatment. The need to regroup medical forces and resources should not increase morbidity or mortality from diseases other than COVID-19.